Project
Background
More than 25% of patients referred for diagnostic coronary angiography and percutaneous coronary intervention (PCI) due to acute coronary syndrome (ACS) suffer from non-valvular atrial fibrillation (AF). In this particular setting, balancing between the prevention of thrombosis and the risk of bleeding remains challenging. Oral anticoagulation (OAC) prevents stroke and systemic embolism but does not prevent stent thrombosis. Dual antiplatelet therapy (DAPT) reduces the incidence of recurrent ischemic events and stent thrombosis but is less effective in reducing the incidence of cardioembolic stroke associated with AF. A common guideline-supported practice is to combine all three drugs (OAC, aspirin, and clopidogrel) in triple therapy, but this approach remains an expert opinion. Moreover, triple therapy is associated with a high annual risk (up to 25%) of major bleeding. Thus, new therapeutic strategies are urgently needed to maintain efficacy while improving treatment safety in patients with AF and ACS undergoing PCI. We hypothesize that dual antithrombotic therapy, including reduced dose ticagrelor (study group, n=1115), is non-inferior regarding bleeding risk and ischaemic protection to the standard triple therapy (control group, n=1115) in patients with AF and treated with PCI due to ACS.
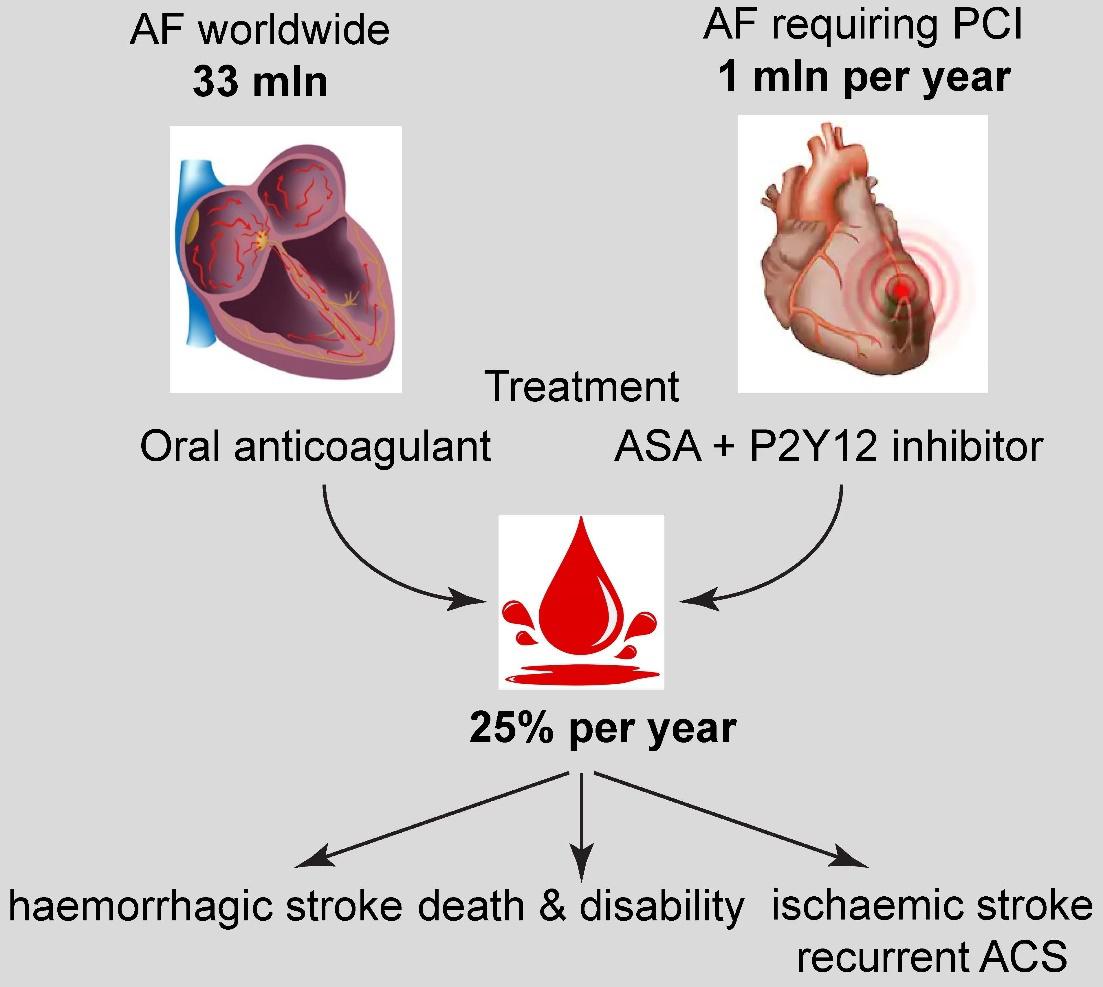
Figure 1. Therapeutic problem: triple therapy in patients with atrial fibrillation (AF) undergoing percutaneous coronary intervention (PCI) is associated with the high rate of bleeding (up to 25% per year). Novel therapeutic strategies are urgently needed to decrease the bleeding risk while maintaining the efficacy of treatment in this specific population.
Study population
The study’s target population is male and female patients aged ≥18 years with non-valvular AF that underwent a successful PCI due to an ACS. AF may be paroxysmal, persistent or permanent but must not be secondary to a reversible disorder such as myocardial infarction, pulmonary embolism, recent surgery, pericarditis, or thyrotoxicosis. ACS may be ST-elevation myocardial infarction (STEMI), non-STEMI (NSTEMI), or unstable angina (UA).
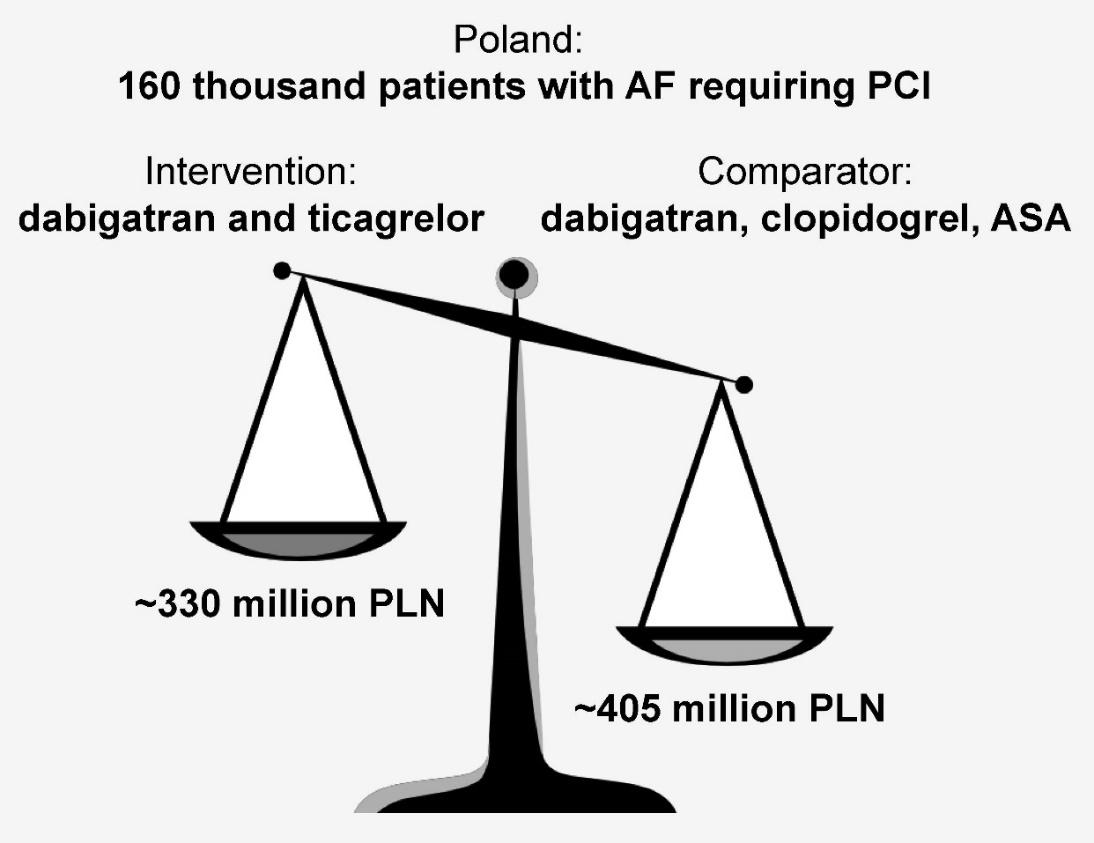
Figure 2. Cost estimation of the interventional treatment (intervention) and standard treatment (comparator), taking into account (i) the extra cost of ticagrelor, and (ii) the spared cost due to the 10% reduced rate of major bleeding on interventional treatment.
Study design
This is a multicentre, prospective, randomized, open-label, blinded endpoint, non-inferiority trial. Within 72 hours post PCI, patients will be randomized in a 1:1 ratio to receive one of the two treatments: dual therapy with ticagrelor (90 mg twice daily for one month, followed by 60 mg twice daily up to 12 months) plus dabigatran (150 mg twice daily or 110 mg twice daily; standard of care) or triple therapy with clopidogrel (75 mg once daily) plus aspirin (75 mg once daily) plus dabigatran (150 mg twice daily or 110 mg twice daily), according to current guidelines. Study treatment will be continued for 12 months.
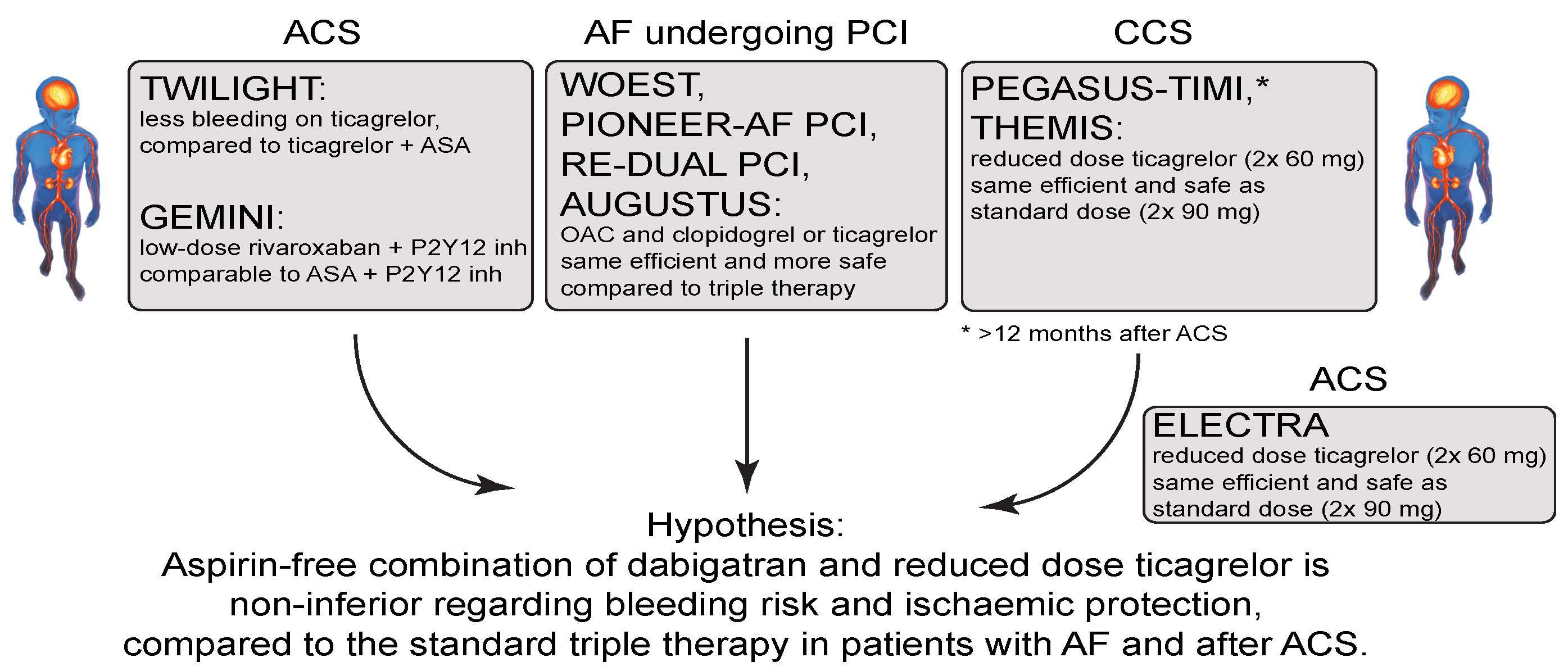
Figure 3. Hypothesis of the study.
Endpoints
The primary study endpoint is the first major or clinically relevant non-major bleeding event, as defined by the International Society on Thrombosis and Haemostasis (ISTH), in a time-to-event analysis. The main secondary endpoint is a composite efficacy endpoint of thromboembolic events (myocardial infarction, stroke, or systemic embolism), death, or unplanned revascularization (PCI or coronary artery bypass grafting).
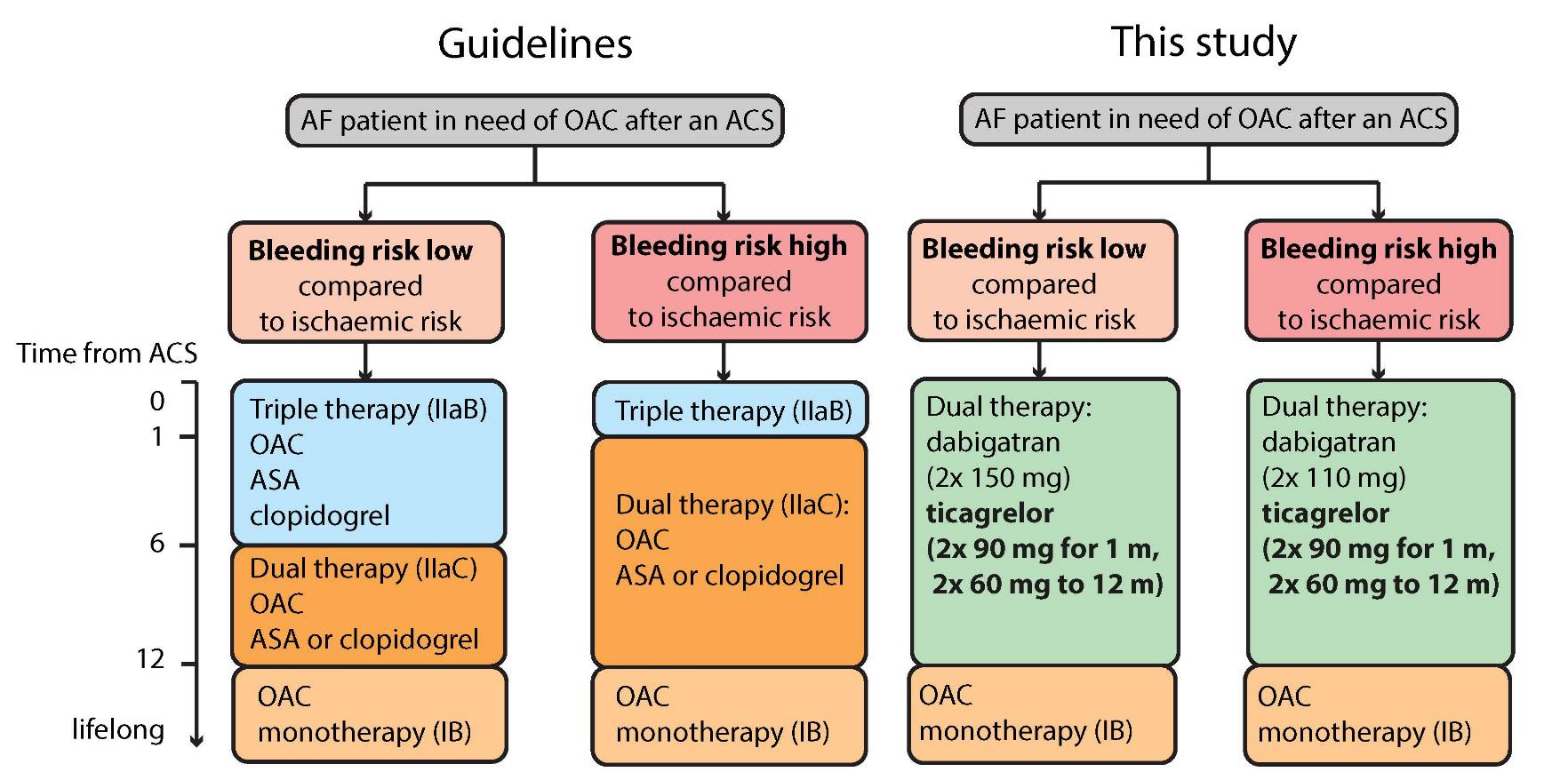 Figure 4. The comparison between the indications and treatment regimen recommended in the guidelines and proposed in this study is presented in Figure 5.
Figure 4. The comparison between the indications and treatment regimen recommended in the guidelines and proposed in this study is presented in Figure 5.
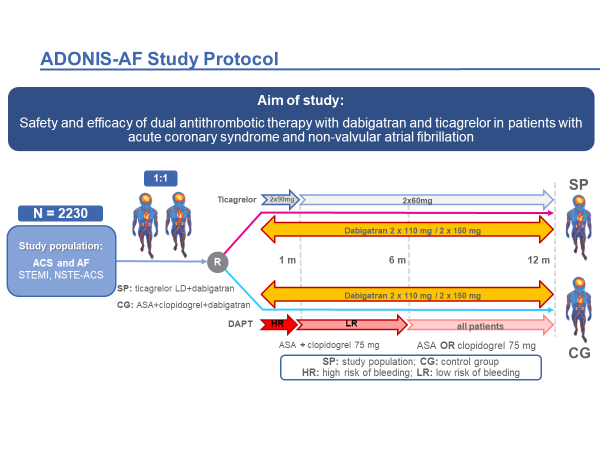
Figure 5. Study design.
Expected results
We expect that the off-label regimen of dual antithrombotic therapy, including reduced dose ticagrelor, is at least non-inferior regarding bleeding risk and ischaemic protection, to the standard triple therapy in patients with AF and after ACS, treated with PCI.
Discussion
We propose a new off-label treatment regimen which is reduced dose ticagrelor in patients with AF and ACS. The most scientifically valuable points of the proposed project are the first-ever (i) attempt to administer the off-label potent P2Y12 inhibitor (ticagrelor) as a part of dual antiplatelet therapy in patients with AF and ACS and (ii) evaluation of the reduced dose of ticagrelor in the setting of ACS. The three most innovative aspects are: (i) new treatment regimen with a reduced ticagrelor dose in ACS setting, (ii) possibility to introduce the polypill containing ticagrelor and dabigatran to the Polish market, and (iii) potential manufacture of the polypill containing various doses of ticagrelor and dabigatran, depending on the patient’s individual ischaemic and bleeding risk. If successful, the proposed study will answer the burning clinical question about the optimal treatment strategy in patients with AF and ACS.
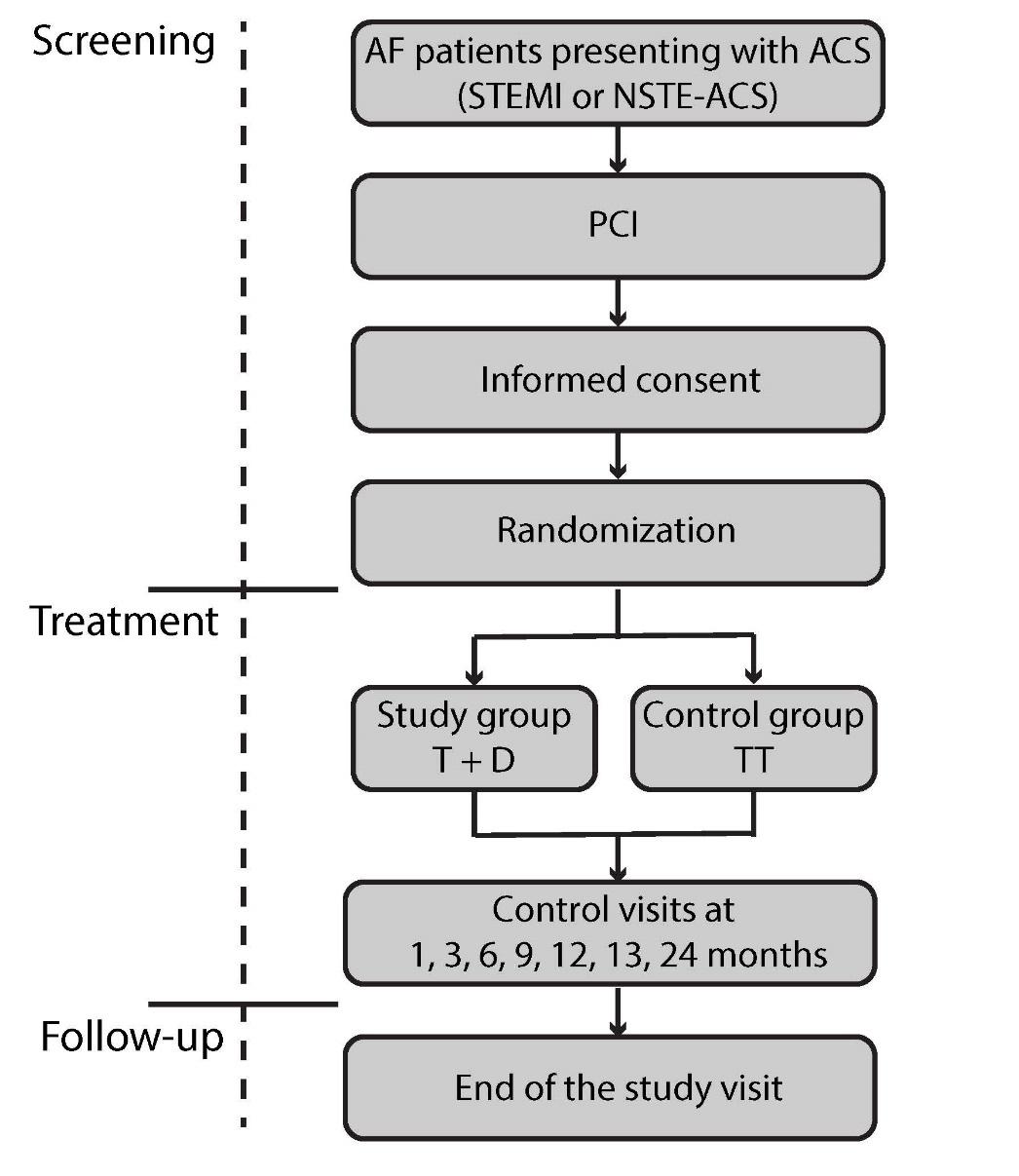
Figure 6. Patient flow.